Periodontal Treatment / Gum Disease
Understanding Periodontal Disease
Periodontal disease is one of the most common infectious diseases globally and one of the leading causes of tooth loss in adults. In fact, almost 90% of the population will present a form of gum disease at some stage of their lives. The good news is, only approximately 15% of people will develop a more advanced condition, which may lead to tooth loss.
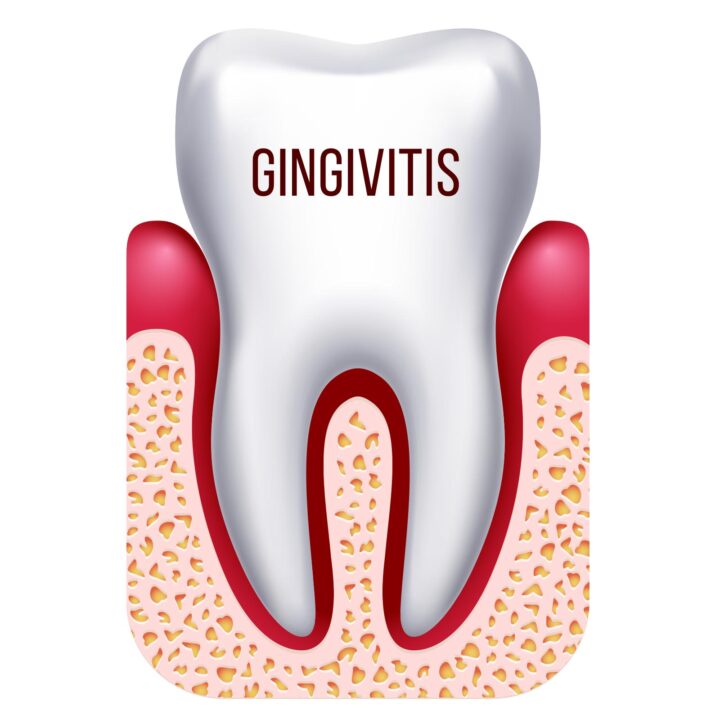
Gingivitis is the inflammation of the gums that occurs when dental plaque is not correctly removed by correct oral hygiene (through tooth brushing and flossing). Gingivitis is reversible. However, it may lead to a more serious condition known as periodontitis if it is not treated.
Periodontitis is a more severe and destructive condition in which the gums, bone and ligaments supporting the teeth deteriorate, creating a deep pocket between teeth and gums. If left untreated, it might lead to further damage, the spread of infection and loss of teeth. Unfortunately, periodontitis is not curable or reversible; however, it is preventable, treatable and controllable if diagnosed at an early stage.
Periodontal disease is usually a painless, slow disease. The most common signs of periodontal disease are red, swollen gums, which easily bleed when cleaned with dental floss and toothbrush, bad breath and bad taste and loose or wobbly teeth. The gums may also recede, exposing the teeth roots and increasing the space between the teeth.

Risk factors
Periodontal disease is not contagious through casual contact. However, sharing cutlery, plates and cups, or kissing someone who has gum disease over a long period, may increase your chances of developing this condition.
Although inflammation due to bacterial infection is behind all forms of periodontal disease, various factors can influence the severity of the disease. In general, the risk factors associated with Periodontal Disease are:
Genetics;
Ageing;
Smoking and tobacco use;
Alcohol consumption;
Drugs abuse;
Crooked, crowded and misaligned teeth;
Compromised tooth fillings and crowns;
Food impaction;
Chewing forces and bite problems;
Clenching and grinding of the teeth;
Poor salivation and dry mouth;
Poor oral hygiene (plaque accumulation & calculus formation).
Smoking is a major risk factor for periodontitis and the severity of the condition. Smokers are three times more likely to develop a severe form of periodontal disease and present lower chances for a successful treatment and a higher prevalence of tooth loss. Some research suggests that passive smokers also present higher risks to develop periodontal disease.
Even though the chances to develop periodontal disease increase with age, teenagers may develop the very aggressive disease.

Periodontal Disease and Systemic Health
Various studies have shown the association between periodontal disease with several other health conditions, such as:
- Nutritional deficiency;
- Cardiovascular disease (e.g. stroke, heart attack, high blood pressure and atherosclerosis);
- Rheumatoid arthritis;
- Endocrine disorder (e.g diabetes);
- Hormonal changes (e.g. puberty, pregnancy and post-menopausal);
- Respiratory disease (e.g. COPD, asthma and emphysema);
- Blood disorders (e.g. leukaemia, low platelet level and anaemia);
- Chronic kidney disease (CKD) and Liver condition;
- Osteoporosis;
- Obesity;
- Compromised Immune condition (e.g. AIDS);
- Psychosomatic or emotional disorders (e.g. stress and depressive disorders).
Some medications have also shown a relationship with periodontal disease. Such medications include immunosuppressants (e.g. Cyclosporine), anti-seizure medications (e.g. Phenytoin), anti-depressants (e.g. tricyclic drugs), heart disease and blood pressure medications (e.g. beta-blockers), oral contraceptives, diuretics as well as antihistamine drugs.
Untreated, periodontal disease may also affect pregnancy, increasing the risks of maternal infection, preterm/premature delivery, low birth weight, and preeclampsia.
Studies have linked periodontitis to the worsening of some systemic conditions, such as diabetes, heart disease, and cancer. Therefore, treating periodontal diseases may also help with the management of other chronic inflammatory conditions.
DIABETES
HEART DISEASE
CANCER
Treatment
The periodontal treatment aims to reduce the number of existing bacteria, reduce pocket depth, repair/regenerate bone and surrounding tissues and control the infection through:
- Patient education, training in oral hygiene, and counselling on control of risk factors (e.g. stress, medical condition, smoking, etc.) with an appropriate referral if needed;
- Professional removal of bacterial plaque (biofilm) and calculus by comprehensive, meticulous periodontal scaling and root planing – local anaesthetic is generally used during these procedures to help eliminate discomfort;
- Selective removal of compromised teeth or implants;
- Establish, maintain and improve the patient’s chewing function using a wide variety of occlusal therapy: change of fillings or crowns, use of an occlusal splint, selective occlusal adjustment, replacement of missing teeth, splinting of teeth, etc.
Treatment may need to be completed over several appointments and should not be postponed.
Following successful periodontal treatment, the gum will often shrink, and in some cases, noticeable spaces may appear between teeth.
It is not possible to predict how the gums and bone will heal, and some areas of infection may not respond to scaling and root planning. Therefore, the need for additional treatment may occur (e.g. re-treatment, periodontal surgery, root canal treatment or tooth extraction).
Periodontal surgery may help the dentist explore and properly treat the affected areas. It may also reduce or eliminate periodontal pockets and create an acceptable gingival/bone form that facilitates oral hygiene and periodontal maintenance. Some periodontal regenerative or cosmetic procedures will aim to correct the damages caused by the disease to bone and gums and enhance aesthetics.
Refusal of treatment may increase the risk of complications, including but not limited to pain, swelling, the spread of infection, loss of function, loss of supporting bone and loss of teeth.
Maintenance
Potentially, any patient with a history of periodontal disease can present a relapse of the condition. However, if the disease is treated correctly and the patient maintains outstanding daily oral care and regular maintenance dental visits, tooth loss and periodontal tissue damage can be contained.
Some important information that helps to prevent the recurrence of periodontal diseases are:
- Understanding the causes, course and risk factors of the disease;
- Visit the dentist routinely for check-ups and professional cleaning;
- Brush your teeth at least twice daily;
- Floss every day;
- Have a well-balanced diet;
- Reduce sugar consumption;
- Don’t use tobacco products;
- Keep good overall health (body and mental).
Remember that teeth are meant to last a lifetime. Tooth loss due to gum disease is not an inevitable result of ageing. Even people who are highly prone to develop periodontal disease can prevent or control the disease with effective good oral care and professional guidance and treatment.
Book an appointment at Banora Family Dental & Implants for a professional check-up, assessment of your gum condition and preventive care.
Not all procedures are available or suitable for every patient, and results may vary.
Book an appointment today. Ph 07 5628 3295
Copyright 2025 Banora Family Dental & Implants. All
Rights Reserved.
Website by Ignition Media.
- 07 5628 3295
- reception@banoradentalimplants.com.au
- Shop 8, Tweed Heights Shops 21-25 Amaroo Drive, Banora Point, NSW, 2486
- Mon - Fri, 8:30 to 5pm